As we take stock of what we've accomplished and where we've failed to measure up, I find my scowling mask of medical skepticism falling away. I have to admit that there is so much wonder and mystery that science and medicine still can't explain.- Wonder Abides (NPR)
Monday, December 29, 2014
Faith & miracles
This is a lovely article to read in the spirit of the season. :)
Monday, November 24, 2014
Tips for the residency interview trail
I'm not going to be bashful about this. I'm known to give pretty good advice. Maybe because I'm a slightly anxious person and a perfectionist so I'm always (over)thinking things? (But then again, one could be too anxious and indecisive making him/her a poor go-to person for advice.) I think it's simply because I do my research before and after an event, evaluating whether or not the advice I got was actually helpful and what advice I would give to my future self and to others. Anyway, I've been on the interview trail for 3 weeks now, and I'm almost half way through. I want to share some tips I've thought of along the way:
- Schedule interviews with ample time in between for travel and rest. Back to back interviews (one day after the other) are absolute no-no's in my book. You might think you're a superhero after going through core surgery and core medicine in MS3, but you don't want to risk it for something this important. And if you're thinking, "well I don't really care about one of the interviews," then you why are you going at all?
Friday, November 7, 2014
Just
Our program director pointed out during her orientation presentation that she's not "just" practicing general medicine, she is practicing medicine. Do you ever hear anyone saying, "I'm just going into orthopedic surgery?"
I'm going into internal medicine, planning to dojust general medicine - either as a hospitalist or a PCP or both. :)
I'm going into internal medicine, planning to do
Saturday, November 1, 2014
Taiwan tops the expat health care charts
- The TelegraphNearly seven in 10 expats in Taiwan say they spend less on health care than they used to before moving – compared with a global average of just three in 10.The FCO [Foreign and Commonwealth Office] states in its guide to the country: “As is to be expected of a nation as developed as Taiwan, health care facilities and medical equipment are of outstanding quality. Since 1995, Taiwan has had a socialised health care plan, the National Health Insurance (NHI) which covers nearly all citizens.”
My thoughts: Of course the survey is biased, in particular a lot of selection bias. Its respondents are not randomized, so you don't get a good representation. Also, the more important question is do you get quality health care for your dollars spent, however much less you do have to spend? That was a major debate in the comments section... I wish I had more time to look into this more, but some anecdotal "evidence," I've heard from friends who've spent time in Taiwan that you do get decent healthcare in Taiwan. I don't think anyone can beat the technology and innovation of the U.S., but we already know that U.S. health care system is far from being a model one.
Also, this is another piece of real life evidence that a country can be non-socialist and still have a socialist health care finance structure and not combust into a complete socialist government. So surprising! (Not.)
Saturday, August 2, 2014
Things making me happy this week
- Journaling: it’s so wonderful to indulge in your own mind. It’s like taking a walk after a long day of sitting at a desk. You forget you had such wonderful muscles/thoughts.
- Learning so much from my attendings (my old ICM preceptors…we go way back)…Dr. H and Dr. S have both taught me so much about not just diagnosis and management of specific disorders, but clinical thinking and management. Here are some examples -
- Be mindful of the labs & tests you order: Don’t order a set of labs just because some preceptor at some point taught you to do so, think about whether or not the results would actually change your treatment plan. For hyponatremia, if you have a clinical diagnosis of true hypovolemia causing a hypotonic hyponatremia, then just start a trial of IVF hydration, and see what happens…if they respond, then that confirms your diagnosis! If you actually got labs, and the results point more toward SIADH, then what are you going to do with that information? Give the patient a vaptan or demeclocycline when they’ve already responded to IVF hydration? No.
- Just because a patient’s outside PCP or previous physicians have decided that the patient is at her baseline but she’s clearly still hypertensive or hyperglycemic, don’t just assume this is just her normal. It’s not normal! Don’t give into clinical inertia!
- Anticipatory medicine: even though the bump in creatinine might not be technically acute renal failure (>0.3 increase in Cr, >50% increase in Cr, or UOP <0.5L/kg/hr over <48 hours), doesn’t mean it won’t be by the next AM labs.
- Look at everything in the patient’s clinical context! If the patient is floridly psychotic and/or unstable, you worry more about their mildly abnormal lab values and vitals than if they’re clinically normal and at baseline. You widen your differential to include more rare and scary diagnoses, and order more labs to rule them out.
- Even when I’m at my loneliest and most down-trodden moments, I’m so appreciative of the support and love I have from my friends. Remember that love. Remember all the moments we’ve shared together and will continue to have together and let that give you strength!
- Getting that 7-8 hours of sleep Wednesday night. It’s true. Your brain performs better on more rest than on more information.
Thursday, July 17, 2014
New technologies fuel patient participation and data collection in research
- sciencedaily.com (New technologies fuel patient participation and data collection in research)The changing dynamic of health studies driven by “big data” research projects will empower patients to become active participants who provide real-time information such as symptoms, side effects and clinical outcomes, according to researchers. The analysis lays out a new paradigm for health research, particularly comparative effectiveness studies that are designed to assess which therapies work best in routine clinical practice."When linked to the rest of the available electronic data, patient-generated health data completes the big data picture of real people’s needs, life beyond the health care system, and how changes in health and health care lead to meaningful changes in people’s lives."
My thoughts:
Interesting idea. But still some obvious flaws. Must be some self-reporting bias among other biases... not unlike that of patients rating doctors, clinics, and hospitals... -_-
Lessons Learned Circumnavigating the Globe
"This was the first time that I realized that my own country, where we lament bad health care and florid corruption, could be seen as privileged. No child here has to die from hydrocephalus. That day I realized that the people for whom I advocate are more than the people of South Africa, more even than the people of Africa. As I walked out of the orphanage, all I could think of was how to fix this – this country I had never before seen nor felt particularly drawn towards. In the global village, the disenfranchised of Vietnam – and of any other country – are our compatriots, too."--Lessons Learned Circumnavigating the Globe
The most powerful thing you can do is to simply write about what you know.
Sunday, June 22, 2014
Lessons in Global Health: What Every Student Should Know
- One of the first and most important lessons I learned was that earlier in your career, you will receive far more than you will be able to give.
- Nonetheless, they were still important because they taught me the complexity of navigating research design and protocol in other countries, the uncertainty involved with international endeavors, and the persistence that differentiates those who remain in global health and those who come to visit for a short time.
- They [the patients] sacrificed, not necessarily because they believed it would make a difference in their lives, but rather because in poorer regions of the world, relationships and hospitality are valued sincerely.
- Another important insight I gained only by taking chances was that you are your only limitation.
- One last lesson I learned was that as a student in global health, your biggest contribution will be determined by the greatest need.
Friday, May 9, 2014
The use of sterile maggots in wound management
Learned today that this is a thing. The joys of being on psych consult!
- It’s long been recognized that opportunistic infestations by maggots of wounds sustained in battle can prevent infections or even septicemia
- It was widely used until early 1940s when antibiotics were introduced
- How it works:
- Debridement due to maggots’ production of enzymes including collagenases, chymotrypsin-like & trypsin-like enzymes
- Disinfecting of the wound via their anti-microbial secretions
- Stimulates wound healing possibly by stimulating fibroblasts
- It’s like the super early version of wound vacs…with anti-microbial properties.
Sunday, May 4, 2014
Saturday, May 3, 2014
You know you're supposed to be in medical school when
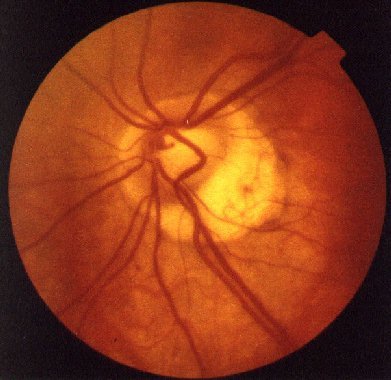
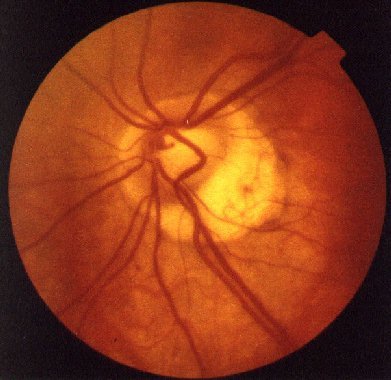
You stay after clinic is over for over an hour to dilate your friend’s eyes, play with the direct and indirect ophthalmoscopes trying to get a good view of her retina, describe your findings…be confused by them, but then have them confirmed by the attending with diagnoses of tilted disc and peripapillary atrophy 2/2 severe myopia. <3
Looked something like this:
Looked something like this:
Friday, May 2, 2014
Wednesday, April 30, 2014
“The doctors, it seemed, never really had enough time for all the patients, try as they might. And over the course of six months, I would corner them in the hallway and ask them a sort of naive, but fundamental question. If you had unlimited resources, what’s the one thing you would give your patients? And I heard the same story again and again, a story we’ve heard hundreds of times since then… ‘Child has an ear infection. I prescribe antibiotics, but the real issue is there’s no food at home. The real issue is that child is living with 12 other people in a two-bedroom apartment, and I don’t even ask about those issues because there’s nothing I can do. I have 13 minutes with each patient. Patients are piling up in the clinic waiting room. I have no idea where the nearest food pantry is, and I don’t even have any help.’”— Rebecca Onie talking about a program she started, Health Leads, that trains college students to help patients find ways to get food, heating, water - basic living requirements allowing doctors at partner institutions (my hospital is one of them!) to give such “prescriptions.”
This is a real problem - as I have seen personally rotating in Baltimore hospitals and clinics. I’m so glad there are programs like these out there. I hope it expands to include many other institutions and/or other people are inspired to do something similar for their hospitals/clinics.
But I would also argue that something else a doctor always wishes he/she could give more of to their patients is time. I’m sure Rebecca Onie also got that answer when she asked her naive, fundamental question to those doctors.
Tuesday, April 29, 2014
“One of the things that I keep going back to over and over again is how do we sensitize clinicians to the patient’s cultural worlds so that we can better understand what’s normal for them and what’s abnormal for them, because only once we’ve done that can we then start to tailor our treatments plans to help our patients in the ways they need in order to lead the lives they want.”— Asian American Mental Health - YouTube project from 4th year psychiatry resident at Columbia
Wednesday, April 2, 2014
“You don’t train someone for all of those years of medical school and residency, particularly people who want to help others optimize their physical and psychological health, and then have them run a claims-processing operation for insurance companies.”— Malcolm Gladwell, from Forbes’ "Tell People What it’s Really Like to be a Physician"
It was really hard picking one section to quote because I loved almost every line of this article. <3 Malcolm Gladwell. Is he married?? Lol, joking.
Sunday, March 2, 2014
On applying to elective opportunities like global health
I really found this inspiring. I love that she found motivation from her grandma. Go grandmas!
I’ll be honest- I didn’t think I had a smidgen of a chance of becoming a Global Health Corps fellow. I had two reactions upon reading the position descriptions and mission statement of GHC. 1) Unprecedented excitement. I knew this was the opportunity I had been looking for, the next step in my career and the chance to actually apply my college education and internship experience into the real world of public health – basically my dream. The combination of fieldwork and professional development, but with an emphasis on fostering a community of leaders dedicated to achieving global health equity, seemed almost too good to be true. This led to thought number 2) Self-doubt. Although on paper I felt qualified for the position I was interested in, and I definitely had the passion and commitment GHC was looking for, I lacked confidence in my ability to persuade the GHC and mothers2mothers teams that I could be the one. Intimidated is an understatement for how I felt while perusing the GHC website. I didn’t have a Masters degree, wasn’t a doctor treating thousands of people on my own, and hadn’t established an NGO at the age of 18. Was I good enough to be one of those smiling faces? Nah, definitely not. Yet, I couldn’t get GHC off my mind. I had to at least make an attempt.
I will admit that I am the Queen of procrastination. I couldn’t bring myself to actually sit down and complete the application. I had the essay topics written on napkins that I tacked over my bed, hoping that I’d get some inspiration in the middle of the night and magically produce acceptance worthy essays. Obviously that did not happen. A week before the application was due, I hadn’t written one word. At this point in time, I had just graduated from George Washington University with an undergraduate degree and was working and traveling around Indonesia. I had a scheduled Skype date with my parents, and as a special surprise, my 92 year-old Grandma joined as well. I excitedly told my family about the GHC application, but as quickly as I lit up about the job posting at mothers2mothers, I followed with a negative remark along the lines of “I’ll never get it-there’s no point blah blah blah woe is me.” My Grandma abruptly shut me up, told me if I didn’t apply she’d disown me, and proceeded to detail all of the reasons why I would be an exceptional candidate. She wouldn’t sign off of Skype until I virtually pinky promised her that I’d apply no matter what. There was something compelling about my Grandma screaming into the computer because she thought being halfway across the world implied that I wouldn’t be able to hear her. Her point came across loud and clear. I signed off after taking an award winning screenshot (see below), went for a surf, and mulled over my options. I could a) not apply, lie to my Grandma, and feel guilty for the rest of my life (this is dramatic but entirely true), b) apply, not become a fellow, but know that I at least gave it a shot, or, c) apply, BECOME A FELLOW, and be one step closer towards pursuing my dreams. A few interviews and one acceptance email later, I became one of the 90 chosen as part of the 2012-2013 GHC fellow class.
Monday, February 10, 2014
Low vitamin D and pregnancy risks
And this just after seeing my preceptor order vitamin D levels on her patients that confuse her because she’s so sure, she rants, that low vitamin D is the culprit whenever something is going on that you otherwise can’t explain…and now this. :)
In the news: Low vitamin D and pregnancy risks (NYTimes)
In the news: Low vitamin D and pregnancy risks (NYTimes)
Sunday, January 12, 2014
Bedside manners
5 Simple Habits Can Help Doctors Connect With Patients http://n.pr/1aNFntJ
- Introducing yourself
- Explaining your role in the patient’s care
- Sitting down (done only 9% of the time! Not surprised.)
- Touching (hand shake, a simple touch on the shoulder)
- Asking open ended questions
Subscribe to:
Posts (Atom)